5 Which of the Following Is a Credentialing Requirement
The accountability framework and decision rights to achieve enterprise info management is known as. The national credentialing requirements for the state of Georgia.
The standards may be minimal and mandatory or above the minimum and voluntary.
. The health center determines its staffing composition for example use of nurse practitioners physician assistants certified nurse midwives and. Primary source verification for provisional credentialing requires only three items. IEHP is required to contract with and credential all Practitioners defined as a PCPs Specialists Non-Physician Practitioners and Physician Admitters including.
Credentialing is simply the activity involved in verifying and the credentials of a physician. Requirements may include establishing competency such as proof of training licensure or certification background checks continuing education hours proof of malpractice insurance coverage and experience working in the field or. Licensure registration accreditation approval certification recognition or endorsement may be used to describe different credentialing processes but this terminology is not applied consistently across different settings and countries.
Although hospital credentialing can typically be done within 90 days in most scenarios it is advisable to give it at least 120 days. The following points describe areas where health centers have discretion with respect to decision-making or that may be useful for health centers to consider when implementing these requirements. Sent to Medical Executive Committee 8.
Similarly annual documentation of your flu vaccine or a waiver for the flu vaccine is required. Information regarding Hepatitis B vaccination as well as MMR measles mumps rubella is required with the initial credentialing application. Documentation must show that the following sites have been queried.
Conforming to all applicable licensing certification or other professional standards as set forth. 1has authority to make final decisions. Credentials Committee of medical Staff Reviews 7.
Sent to Governing Board who decides and grants credentials. Provider credentialing in healthcare is the process by which medical organizations verify the credentials of healthcare providers to ensure they have the required licenses certifications and skills to properly care for patients. Five years of malpractice history.
The requirement for an HIM professional to comply with all laws regulations and standards governing the practice of HIM is in the AHIMA __________. Verified Information sent to department Chairmen for review 6. You may not need the 30 days of extra time but beginning the credentialing process at least 120 days before your start date will provide a cushion for unexpected delays.
This includes education and training board certification if applicable professional licensure DEA malpractice and work history malpractice coverage professional. - It also ensures our patient are getting the best care from providers who are competent and qualified. The process is also called physician credentialing medical credentialing or doctor credentialing.
Subcutaneous and intramuscular injections. The Department of Health Human Services tracks the number of lawsuits 13. A current valid medical license.
Some of the forms of verification usually include but may not be limited to the following. All of the following statements about negligent credentialing are true except. Description of health status 4.
The credentialing process must be in compliance with federal requirements that prohibit employment or contracts with providers excluded from participation under either Medicare or Medicaid. 5 Practitioners who do not provide care for members in a treatment setting eg. The accreditation of an OT program means that the school has received the formal approval of AOTA through ACOTE Accreditation Council of Occupational Therapy.
Be looking exclusively at the requirements of Medical Staff credentialing. The government continued the COVID. Audiologists Chiropractors DCs Clinical Psychologists Licensed Behavioral Analysts Licensed Clinical Social Workers Marriage and Family Therapists Mental Health Counselors Occupational Therapists Ophthalmologists MDs or DOs Optometrists ODs.
16 rows The 2017 Credentialing Requirements were updated for the following provider types. Other standards related to the credentialing process include the following. 2consistent with medical staff criteria.
Start the Credentialing Process Early. The three credentialing processes are. A physician may delegate to a medical assistant the following medical tasks.
Credentialing is the process of verifying the professional qualifications of medical providers and is required by most medical facilities and services including hospitals and health insurance companies. 3must determine which categories of practitioners are eligible candidates. Proof of education and additional training.
Any 3 of the governing body. Conduct that is culpable because it falls short of what a reasonable person would do. Analyzing the providers documents through a credentialing process guarantees that they are both legitimate and up-to-date.
-It is required by the joint commission state and to reduce risk for the hospital. Organization are outside NCQAs scope of credentialing. The following credentialing requirements apply to the use of certificated substitutes in compliance with the California Commission on Teacher Credentialing the Administrators Assignment Manual Section H.
Why is credentials required. Complying with all applicable state and federal laws and regulations licensing and accreditation requirements and federal and state affirmative action requirements. Query NPDB required by law to obtain report from NPDB on all physicians DEA check 5.
A medical assistant is an unlicensed person employed by the physician to whom he or she delegates certain medical tasks. 1 Individual or group practices. Organizational providers to receive a contract includes the following.
Credentialing also assures the patient that they are being treated by providers whose qualifications training. A major differentiator between the accreditation requirements for healthcare provider organizations and healthcare payer entities regarding credentialing is. The criteria listed above apply to Practitioners in the following settings.
It is recommended to provide any further information about any boosters in a timely fashion. 6 Rental network practitioners who provide out-of-area care only and Members are not required or given an incentive to seek care from them. And a current signed application and attestation.
Refers to the credentialing of an institution college or university. The definition of negligent credentialing is. Credentialing is a formal process that utilizes an established series of guidelines to ensure that patients receive the highest level of care from healthcare professionals who have undergone the most stringent scrutiny regarding their ability to practice medicine.
He or she should be advised to submit a provider-enrollment packet specific to that carrier including the required credentials as soon as possible when considering an employment opportunity. Substitute Teaching the California Administrative Code Title 5 Education Sections 80025 80026 and the.

Physician Credentialing Tips Physician Credentialing Revenue Cycle Management Health Information Management Medical Coder
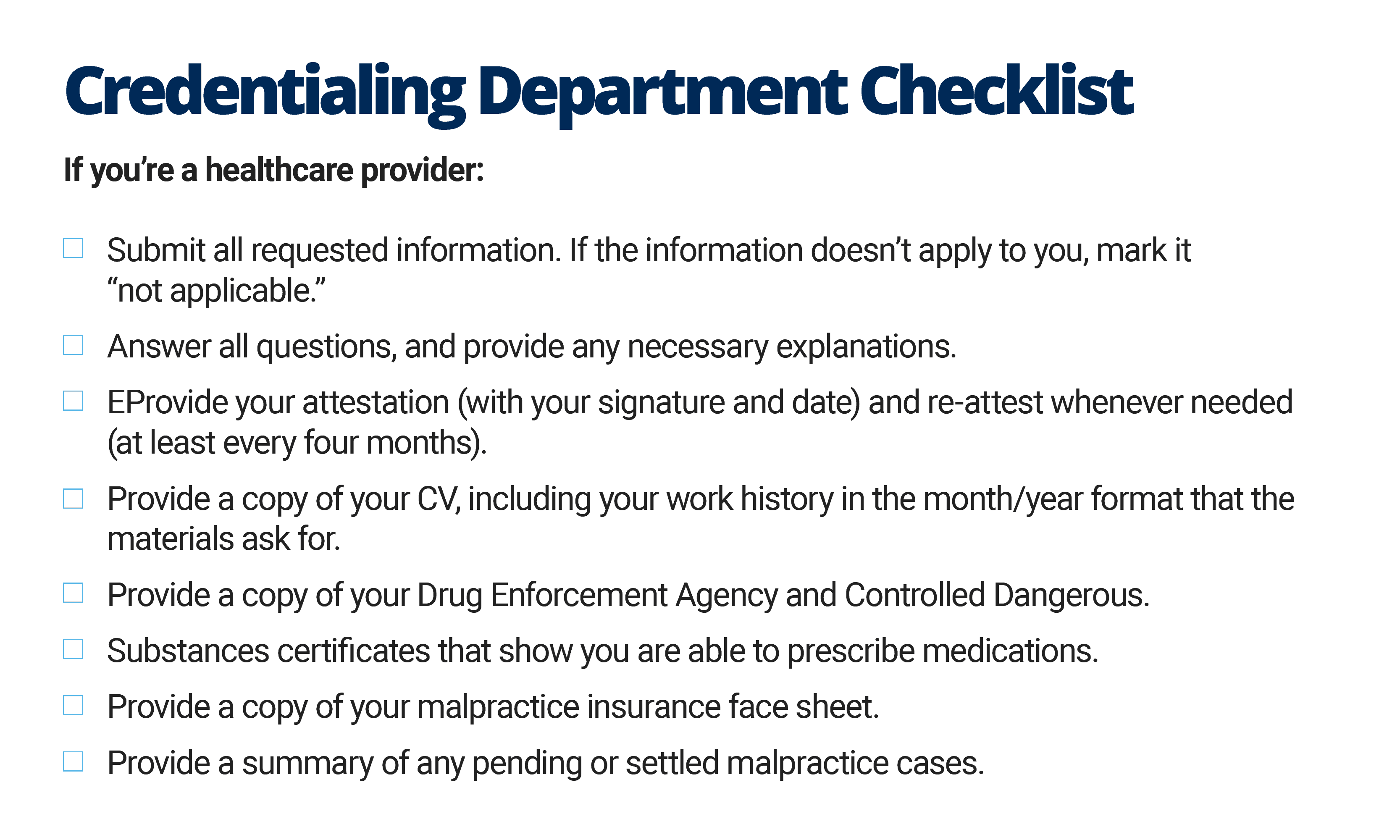
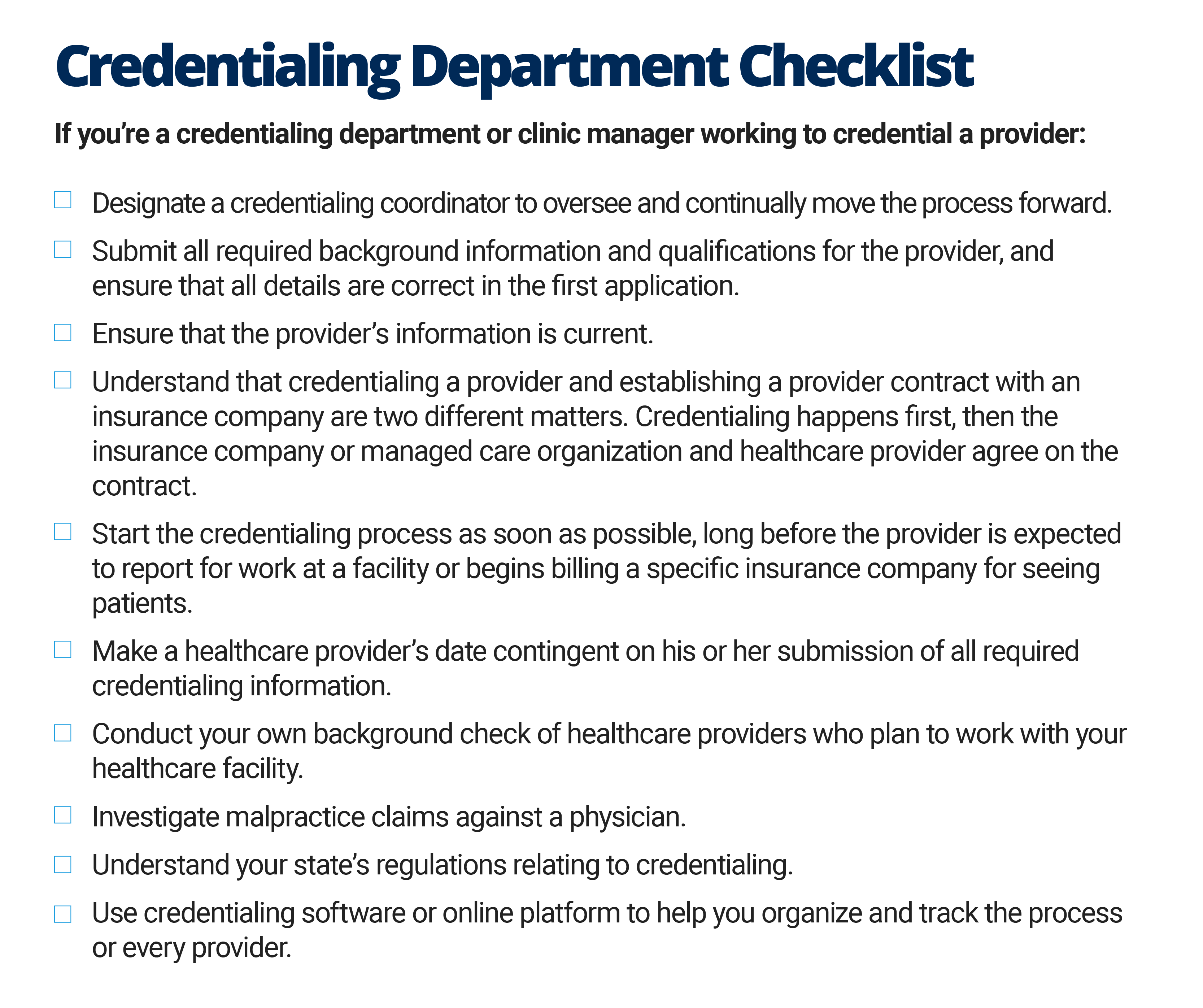
The Quick Guide To Healthcare Provider Credentialing Smartsheet
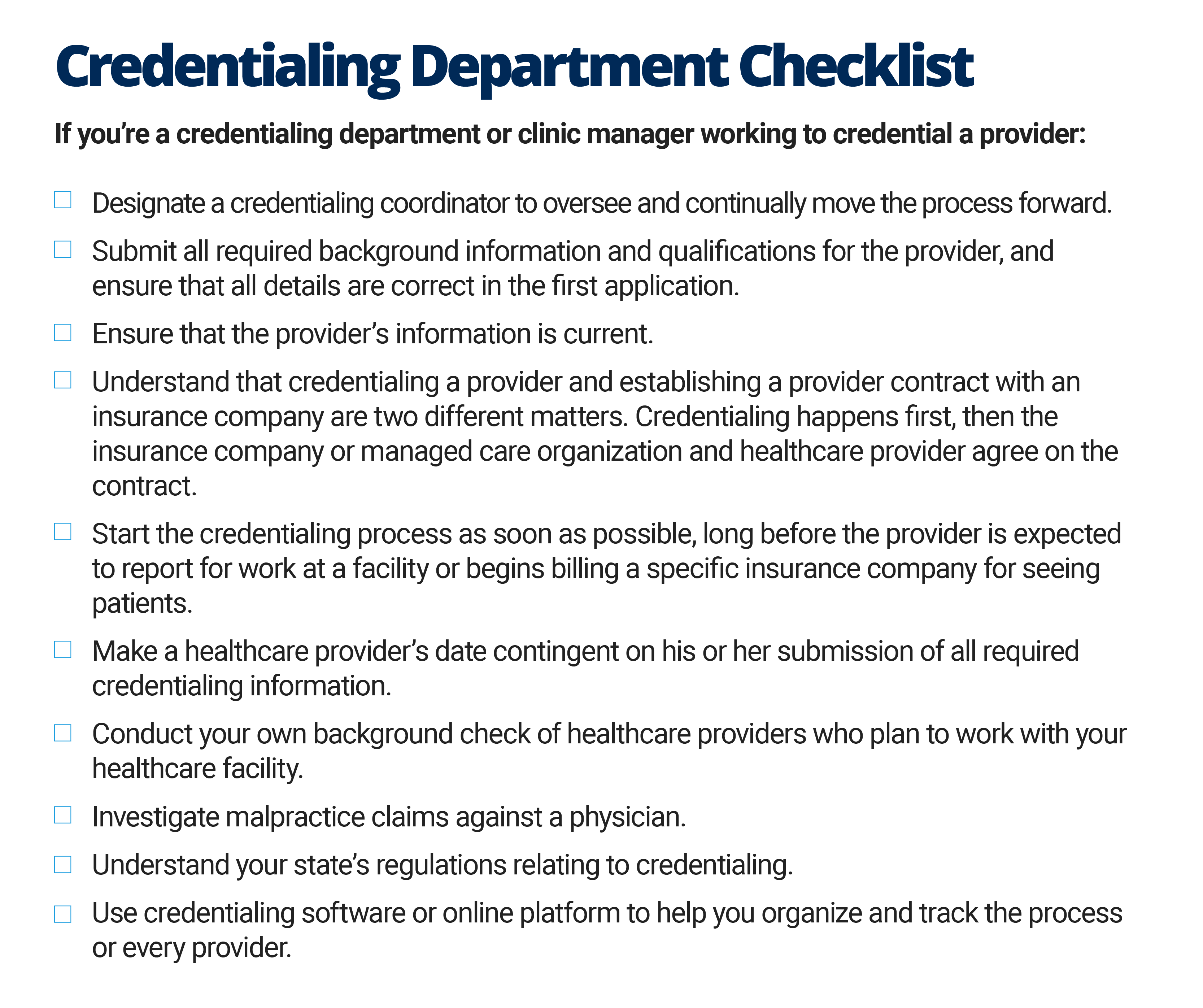
The Quick Guide To Healthcare Provider Credentialing Smartsheet
No comments for "5 Which of the Following Is a Credentialing Requirement"
Post a Comment